Nerve Surgery for Post-Mastectomy Pain Syndrome in Florida
What is Post-Mastectomy Pain Syndrome (PMPS)?
Post-Mastectomy Pain Syndrome (PMPS) is chronic nerve pain that can develop after breast surgery, most commonly mastectomy or reconstruction. Patients often describe it as burning, aching, or shooting pain that radiates from the chest wall to the armpit or upper arm. This pain can surface weeks, months, or even years after surgery and often feels unrelated to healing or scar tissue. PMPS occurs when nerves are damaged during surgery, leading to long-term sensitivity, numbness, or loss of function. While medications, therapy, and injections may offer temporary relief, they typically don’t fix the root cause.
Our Florida surgeons specialize in advanced nerve repair, decompression, and grafting procedures that directly address the source of the pain—giving patients a real chance at lasting relief and restored quality of life.

Check Your Symptoms: Are You Experiencing Any of the Following?
- Burning, shooting, or stabbing pain near your breast, armpit, or chest wall
- Numbness or tingling that lingers long after surgery
- Pain that worsens with movement, deep breaths, or cold weather
- Hypersensitivity to touch—especially along the ribs or underarm
- Limited shoulder or arm mobility
- Ongoing discomfort despite physical therapy or medications
Treatment for PMPS: Do You Know Your Surgical Options?
This procedure relieves pressure on entrapped nerves, reducing hypersensitivity and restoring normal nerve signaling. It’s minimally invasive and often used when scar tissue is causing compression.
When a nerve forms a painful neuroma (a bundle of damaged nerve fibers), surgeons can remove the neuroma and reconnect healthy nerve ends or use grafts to restore function and reduce pain.
If a nerve has been severed or significantly damaged, grafting bridges the gap using donor nerve tissue. This can restore sensation and reduce chronic pain over time.
TMR involves rerouting severed nerves to nearby muscles to prevent neuroma formation and reduce phantom or residual pain. This is particularly effective for patients with significant nerve disruption.
These implants create a scaffold that supports nerve regeneration across gaps. Often combined with repair or grafting techniques, they can improve healing outcomes and functional recovery.
Find Out If You’re Eligible for PMPS Surgery in Florida
See How We’re Changing Lives, One Patient at a Time
Benefits of Surgery
Am I a Candidate for Surgery?
If you’re still in pain months after your mastectomy or reconstruction, and non-surgical treatments haven’t helped, nerve surgery may be the next step. Our specialists evaluate each case individually to determine if your symptoms stem from treatable nerve damage.
You may qualify if you have:
- Burning, stabbing, or aching pain near the breast, armpit, or upper arm
- Pain that hasn’t improved with physical therapy, injections, or medication
- Hypersensitivity to touch in the chest wall or underarm
- Confirmed or suspected nerve injury from breast surgery


Why is Post-Mastectomy Pain Syndrome Often Misdiagnosed?
Post-Mastectomy Pain Syndrome is often overlooked because its symptoms are easily mistaken for post-surgical healing or scar sensitivity. Many patients begin with first-line treatments such as medication, injections, or physical therapy, but when those approaches don’t resolve the pain, it may point to an underlying nerve injury. Our Florida nerve specialists have the specialized expertise to identify and treat these overlooked nerve issues—helping patients finally find answers and long-term relief.

Considering Surgery for Post-Mastectomy Pain? What to Expect:
Precision Diagnostics
We use a combination of detailed physical exams, patient-reported symptom mapping, and diagnostic nerve blocks to pinpoint the exact source of pain. This ensures that only patients with confirmed nerve injury move forward to surgery—reducing unnecessary procedures and improving outcomes.Tailored Surgery
Our surgeons perform nerve decompression, neurolysis, and grafting procedures using high-powered surgical magnification and microsurgical instruments designed for delicate nerve work. In some cases, image guidance and intraoperative nerve monitoring are used to maximize precision and protect surrounding structures.Rapid Recovery
Most nerve surgeries for PMPS are outpatient procedures performed under general anesthesia. Patients typically resume light activity within 1 to 2 weeks, with full nerve regeneration occurring gradually over several months. Compared to more invasive breast or reconstructive surgeries, recovery from nerve procedures is generally shorter, with fewer restrictions and a faster return to daily life.Why Trust The Institute of Florida?
One of the Few U.S. Centers Specializing in Surgical Treatment for Post-Mastectomy Pain Syndrome
We are a national referral destination for breast cancer survivors suffering from chronic nerve pain after mastectomy or reconstruction. Our surgeons perform one of the highest volumes of nerve decompression procedures for PMPS—delivering unmatched experience in both diagnostics and repair.
Surgical Expertise That Begins With the Nerve
We treat the root cause of PMPS—damaged or entrapped intercostal nerves—using techniques like neurolysis, nerve grafting, and decompression. Our team includes board-certified microsurgeons with extensive training in surgically induced neuropathic pain.
Technology Designed for Precision Nerve Repair
We use high-magnification optics, intraoperative nerve monitoring, and specialized microsurgical instruments to safely release nerves and restore normal signaling—without compromising surrounding tissue.
More than 80% of Patients Report Lasting Relief
We measure more than procedures—we measure outcomes. Over 80% of our PMPS patients experience significant pain reduction and improved quality of life after surgery, even after failed conservative care.
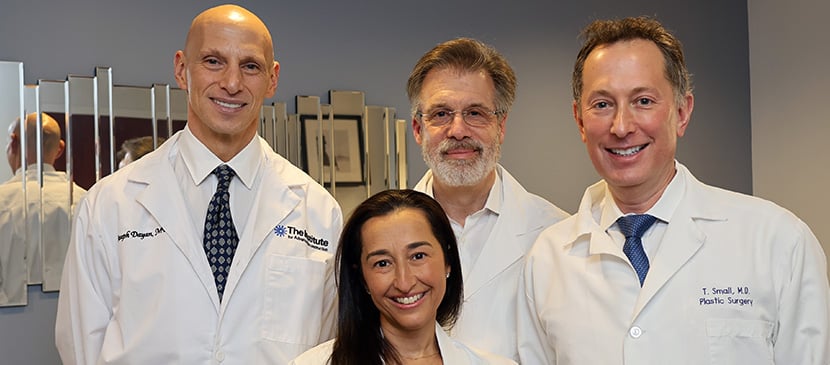
Meet Florida’s Top
Nerve Surgery Experts

Plastic & Reconstructive Surgeon
Board Certified in Plastic Surgery
Still in Pain? Let’s Fix That.
If you’re living with unresolved post-mastectomy pain—or treating a patient who is—our team is here to help. With advanced surgical expertise and proven results, we offer real hope for lasting relief.
Now seeing patients in Ft. Lauderdale and Boynton Beach.
Frequently Asked Questions
PMPS is a form of chronic nerve pain that can develop after a mastectomy or breast reconstruction. It’s often felt as burning, tingling, or sharp pain near the chest wall, armpit, or upper arm and may appear long after surgical healing.
Ongoing breast or chest pain years after surgery is often linked to undetected nerve injury. This pain doesn’t always show up on scans or respond to medication—but may be treatable with nerve surgery.
Pain in this area is frequently due to intercostal nerve entrapment or scarring near the surgical site. These nerves can become compressed or damaged during mastectomy or lymph node dissection, leading to long-term discomfort.
As with any surgery, risks include bleeding, infection, or nerve sensitivity. However, our procedures are typically outpatient and performed with microsurgical precision to reduce complications and protect surrounding tissue.

.jpg?width=1280&height=720&name=maxresdefault%20(5).jpg)

.webp)



